Otezla Appeal Letter Template

0 co pay program the majority of people pay nothing out of pocket for otezla with the 0 co pay program.
Otezla appeal letter template. The otezla letter of medical necessity is provided to assist with appealing a coverage denial for an otezla prescription. Help with insurance questions any insurance coverage help or assistance in working with a specialty pharmacy to get your otezla. To receive a letter of medical necessity by fax or if you have any questions call otezla supportplus at 1 844 4otezla 1 844 468 3952. An authorization letter is issued by an individual company or business concern in order to invest the recipient with certain powers which can be anything from withdrawing money from a bank account to making a business deal.
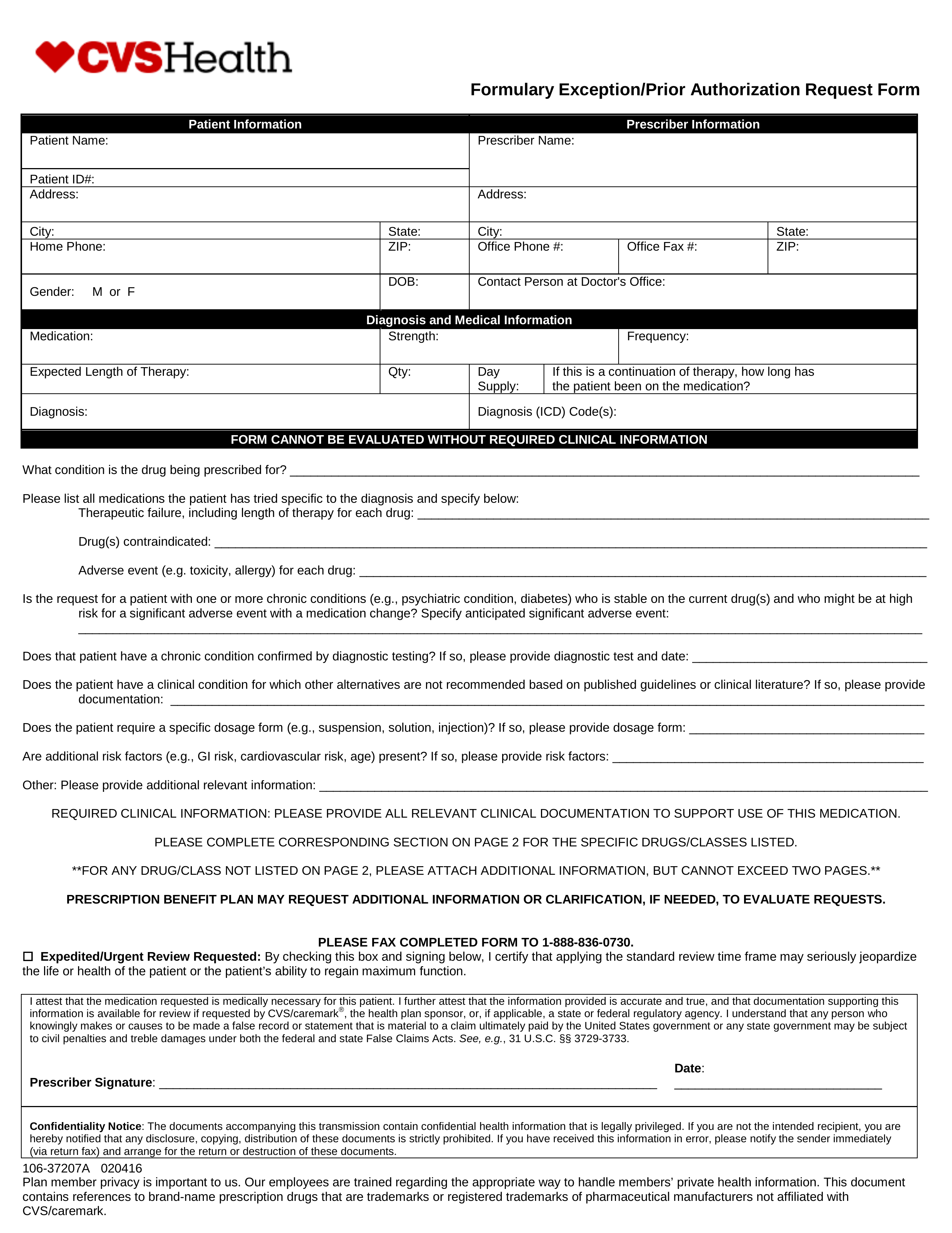
If a coverage appeal is still denied refer the patient to otezla supportplus to determine eligibility for the patient assistance program. The following graph will help you get your patients started on otezla. 7 sample letter of medical necessity. Obtain guidance and documents for patient assistance programs and educational materials to help patients stay on treatment track symptoms and enhance discussions with healthcare providers.
Authorization letters are documents which transfer power from one person to another even if only as a token or in a nominal manner. The otezla bridge program if you have private insurance and are experiencing delays or your private insurance doesnt cover. Tell us a little about yourself and a patient navigator will get. Prescription enbrel is administered by injection enbrel is indicated for reducing signs and symptoms inducing major clinical.
Sample prior authorization appeals letter from patient and physician this type of letter may be used when a prior authorization request has been denied. What happens if the otezla letter of medical necessity has been denied. Request this document on the letter of medical necessity page. Provide you and your physician with template letters to help you be successful in your insurance appeal.
They may already be working with your doctor to appeal the insurance companys denial letter. Appeal the denial by submitting the letter of medical necessity and other required documentation to the insurer. 3 when a prior authorization or formulary exception request is denied you can submit an appeal. Content on this page does not need to be sent to the insurance company.
What you get with supportplus. The resource center provides instructions and forms to prescribe otezla apremilast. Well share the appropriate template appeal letters and guide you through the appeals process.